What is Diabetic Retinopathy Treatment?
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye. High blood sugar levels can damage these blood vessels, causing them to swell, leak, and eventually close, leading to vision problems.
In severe cases, the eye may try to grow new blood vessels to compensate for the damage, but these new blood vessels are often weak and can bleed easily.
Initially, you don’t experience any symptoms; however, if left untreated, diabetic retinopathy can cause blindness. It is a dangerous eye problem because it is irreversible, and it is difficult to restore the lost vision. In this guide, we will explore the causes, symptoms, stages, diagnosis, and diabetic retinopathy treatment in detail.
Let’s get started!
Diabetic Retinopathy
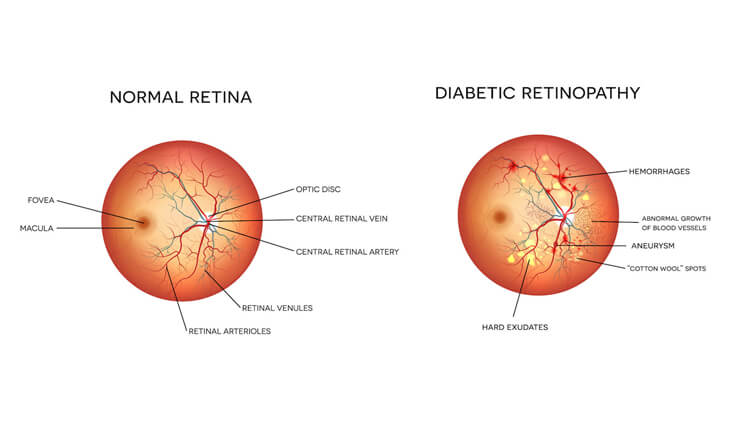
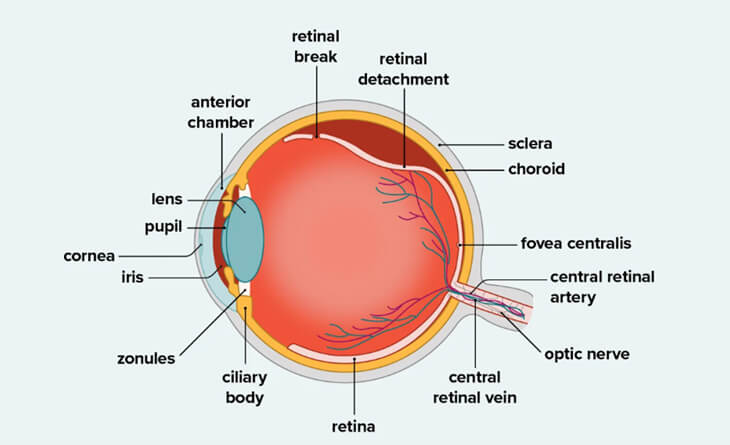
The retina is the light-sensitive tissue that lines the back of the eye. It converts light into electrical signals that are sent to the brain, where they are interpreted as images.
In diabetic retinopathy, high blood sugar levels block the small blood vessels, leading to the formation of abnormal blood vessels that leak fluid or blood. If this fluid or blood collects in the macula, the central part of the retina, it can cause blurred vision that requires treatment.
As the disease progresses, larger blood vessels may become blocked, preventing the retina from receiving enough oxygen and nutrients. This can lead to the growth of new abnormal blood vessels, called neovascularization. These new blood vessels are fragile and prone to leaking and bleeding, which can cause blood in the eye, scarring, and further damage to the retina. In advanced cases, this can lead to retinal detachment.
People with both type 1 and type 2 diabetes are at risk of developing diabetic retinopathy, and the risk increases with the duration of diabetes. They may require invasive diabetic retinopathy treatment such as surgery or injections.
Cause of Diabetic Retinopathy
High blood sugar levels are the major cause of diabetic retinopathy. Diabetes can damage the small blood vessels in the eye, causing them to thicken, leak, clot, close off, or develop balloon-like defects. This can lead to fluid buildup in the retina, resulting in vision problems such as blurry vision, eye bleeding, and retina separation from the back of the eye.
Areas of the retina with damaged blood vessels produce vascular endothelium growth factor (VEGF) that promotes the growth of new blood vessels. However, these new blood vessels are abnormal and can bleed, causing vision loss. Additionally, fluid buildup in certain areas of the retina, especially the center (macula), can lead to direct vision loss.
Risk Factors Associated with Diabetic Retinopathy
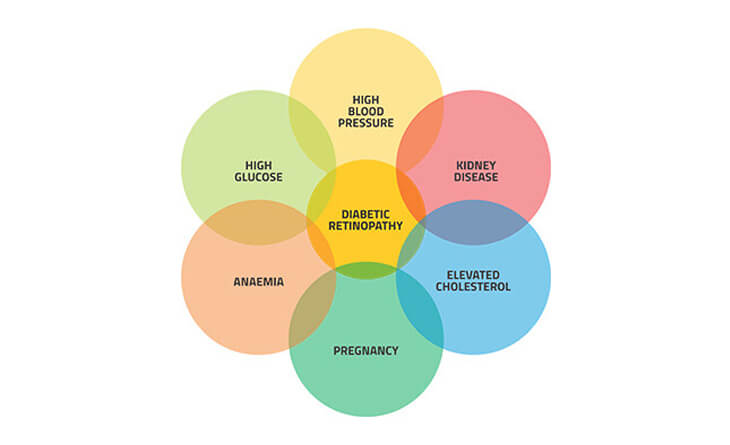
The main risk factors for diabetic retinopathy may include high blood sugar levels, high blood pressure, high lipid levels, duration of diabetes, age, and genetic predisposition.
High Blood Pressure: High blood pressure can cause retinal blood vessel injury. When blood pressure is elevated, the force of the blood against the blood vessel walls increases. This can cause damage to the blood vessel walls, increasing the likelihood of leakage or closure.
High Cholesterol Levels: High cholesterol levels can also damage blood vessels. Lipids can accumulate on the walls of blood vessels, restricting them and making blood flow more difficult. This can result in blood vessel damage and eyesight issues.
Genetic Factors: Some people may be more genetically predisposed to developing diabetic retinopathy than others.
Duration of Diabetes: The risk of developing diabetic retinopathy increases with the longer you have diabetes. People who have had diabetes for more than 10 years are more likely to develop diabetic retinopathy.
Pregnancy: Women with diabetes who have a healthy retina at the beginning of their pregnancy have a low risk of developing diabetic retinopathy. However, women with retinopathy before pregnancy may experience worsening of the condition due to changes in the retina that occur during pregnancy.
A complete diagnosis with an eye specialist can help you find the exact cause and diabetic retinopathy treatment.
Symptoms of Diabetic Retinopathy
In the early stages of diabetic retinopathy, there may be no symptoms because the damage to the blood vessels in the eye is usually not severe enough to cause trouble with your vision. Therefore, it is difficult to detect if you have diabetic retinopathy. As the condition progresses, you may experience the following symptoms:
Blurred Vision: Blurred vision is the most common symptom of diabetic retinopathy caused by swelling in the retina or bleeding into the vitreous, the gel-like substance that fills the inside of the eye.
Dark Spots Floating in Your Vision (Floaters): These are small, dark spots or cobweb-like shapes that float in your vision. They are caused by blood or other debris collecting in the vitreous.
Vision Changes: You may have difficulty seeing at night, reading or focusing on close objects, or experiencing changes in your colour vision.
Vision Loss: This is the most serious symptom of diabetic retinopathy and can lead to blindness. Vision loss can be caused by bleeding in the vitreous gel, damage to the macula, or retinal detachment.
Other signs of diabetic retinopathy:
Eye Pain: In very advance cases of proliferative retinopathy, you can experience eye pain due to a significant increase in the pressure inside your eye caused by large bleeds. This condition is called neovascular glaucoma and is a very dangerous condition.
Microaneurysms: These are the tiny bulges in the blood vessels of the retina that are the first and mildest signs of diabetic retinopathy.
Intraretinal hemorrhages: Intraretinal hemorrhages are small amounts of bleeding from damaged blood vessels in the retina that cause vision loss.
Lipid Accumulation: Fat accumulations caused by leaky retinal blood vessels.
Macular Edema: Fluid leaking from broken blood vessels causes retina swelling.
Vitreous Haemorrhages: Significant bleeding within the vitreous cavity due to retinal neovascularization.
Understanding these signs and symptoms can help you and your doctor to find the appropriate diabetic retinopathy treatment plan.
Complications of Diabetic Retinopathy
As the condition progresses, it can lead to the following serious eye problems:
- Vitreous Hemorrhage: When new blood vessels in the eye bleed into the vitreous, the clear, jelly-like substance in the center of the eye, it can cause floaters or even complete vision loss in severe cases. However, vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks or months, and vision returns to normal unless the retina is damaged.
- Retinal detachment: The new blood vessels that grow in diabetic retinopathy can cause scar tissue to form. This scar tissue can pull the retina away from the back of the eye, causing floaters, flashes of light, or severe vision loss.
- Glaucoma: Abnormal blood vessels can grow in the front part of the eye (iris) and block the normal drainage of fluid, increasing the pressure in the eye. This pressure can damage the optic nerve, which carries images from the eye to the brain.
- Blindness: If diabetic retinopathy, macular edema, or glaucoma are not well-managed, they can lead to complete vision loss.
Diabetes does not always lead to vision loss. By taking an active role in managing your diabetes, you can significantly reduce your risk of complications.
Diagnosis and Prevention of Diabetic Retinopathy
Diabetic Retinopathy is a serious complication of diabetes. Therefore, it is essential to get a comprehensive eye exam once a year, especially if you have diabetes. A complete diagnosis can help your eye doctor to customize the diabetic retinopathy treatment plan based on the severity of the condition.
Diagnosis
Diabetic retinopathy can be a challenging condition. It can sometimes go completely silent, with no symptoms at all. It can harm the peripheral retina without affecting the center or macula, so you may not even know you have it. That’s why you should get regular eye exams if you have diabetes.
If you have type 2 diabetes, you should get screened once a year starting from the day you are diagnosed. If you have type 1 diabetes, you should begin yearly screening 5 years after diagnosis, but try to get your retina checked once a year anyway.
Your doctor may recommend the following test to determine the extent of the condition:
- Dilated eye exam
- Angiography
- Optical Coherence Tomography (OCT)
Prevention
Diabetic retinopathy is a non-reversible condition, so it is difficult to prevent. However, taking a few steps can help prevent severe vision loss.
The most effective way to prevent diabetic retinopathy is to control its underlying causes. So try to keep your blood sugar levels, blood pressure and cholesterol under control. Because if you don’t regulate your sugar level, the problem will return regardless of the diabetic retinopathy treatment.
Follow the below tips to reduce your risks of diabetic retinopathy:
- Take a Healthy Diet: Eat a well-balanced diet that contains whole grains, fruits and vegetables and avoid processed foods, sugary drinks, and saturated and unhealthy fats to keep your blood pressure and cholesterol levels under control.
- Exercise Regularly: Aim for at least 30 minutes of moderate-intensity exercise like walking, swimming and dancing each week.
- Monitor Your Blood Sugar Level: You may need to check your blood sugar several times daily, especially if you are sick or stressed. Talk to your doctor about how often you need to test your blood sugar.
- Quit Smoking: Smoking increases your risk of diabetic retinopathy and other complications of diabetes. Therefore, quit smoking.
- Take Your Medication Regularly: Take your diabetes, blood pressure and cholesterol medications as your doctor prescribes. Don’t skip doses or stop taking your medicines without talking to your doctor first.
- Maintain a Healthy Weight: Being overweight or obese can also increase your complications of diabetes, including diabetic retinopathy. If you are overweight or obese, eat healthy food and exercise regularly to maintain a healthy weight.
- Get Regular Eye Exams: If you have diabetes, get a comprehensive dilated eye exam at least once a year. This allows your eye doctor to see the signs of diabetic retinopathy.
- Pay Attention to Vision Changes: If you notice sudden changes in your vision, spots or haziness, contact your eye specialist in Delhi immediately.
Properly diagnosing and controlling your underlying causes can reduce your risk of vision loss due to diabetic retinopathy.
What are the stages of diabetic retinopathy?
Diabetic retinopathy is a progressive eye disease that worsens over time. This is because the damage to the blood vessels in the retina cannot be reversed.
Diabetic retinopathy is classified into two types: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR), and four stages: mild nonproliferative diabetic retinopathy (NPDR), moderate nonproliferative diabetic retinopathy (NPDR), severe nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
Let’s understand these stages in detail.
Stage 1: Mild NPDR: The earliest stage of diabetic retinopathy is called mild NPDR, or non-proliferative diabetic retinopathy, in which tiny bulges called microaneurysms develop in the retina’s blood vessels. These microaneurysms can leak small amounts of blood and fluid into the retina, worsening the swelling of the macula, the central part of the retina responsible for sharp vision.
In the early stages of mild NPDR, you may not notice any symptoms, so you may not need diabetic retinopathy treatment.
Stage 2: Moderate NPDR: At the second stage of non-proliferative diabetic retinopathy (NPDR), the blood vessels in the retina swell more, interfering with blood flow and preventing the retina from receiving proper nourishment.
While mild NPDR is characterized by at least one microaneurysm, moderate NPDR involves multiple microaneurysms. At this stage, you may start experiencing symptoms such as blurry vision because blood and other fluids accumulate in the macula.
According to the study, the probability of a person with moderate NPDR progressing to severe NPDR or PDR within 5 years of diagnosis is 17.6%.
Stage 3: Severe NPDR: As the condition advances, it blocks the larger sections of blood vessels in the retina. This causes a significant decrease in blood flow to the retina, which prompts the body to grow new blood vessels. These new blood vessels are extremely thin and fragile and can leak blood and fluid into the retina, causing blurry vision, dark spots, and patches of vision loss.
Stage 4: Proliferative Diabetic Retinopathy (PDR): Proliferative diabetic retinopathy (PDR) is the most advanced stage of diabetic retinopathy, and it occurs when the blood vessels in the retina are so damaged that they cannot supply enough oxygen to the retina.
This causes the retina to grow new blood vessels, but these new blood vessels are fragile and can leak blood and fluid into the vitreous, the gel-like fluid that fills the back of the eye.
The leaking blood and fluid can cloud vision and cause floaters, which are dark spots or lines that float in your field of vision. The new blood vessels can also form scar tissue, pulling the retina away from the back of the eye (retinal detachment). Retinal detachment is a serious condition that can lead to blindness if not treated promptly.
If left untreated, PDR can increase the risk of severe vision loss and blindness.
To diagnose the stage of diabetic retinopathy, your doctor will perform an eye exam by placing eye drops into your eyes. This allows your doctor to see the inside of your eye more clearly, including the retina, blood vessels, and optic nerve. Based on the exam findings, the doctor will advise the person on how often they need to be monitored and whether they need any diabetic retinopathy treatment.
What Are the Investigations or Tests for Diabetic Retinopathy?
Diabetic retinopathy can be diagnosed with the following methods:
Visual Activity Testing: This test measures how sharp your vision is at both close and long range. It can be used to detect vision loss and other eye problems.
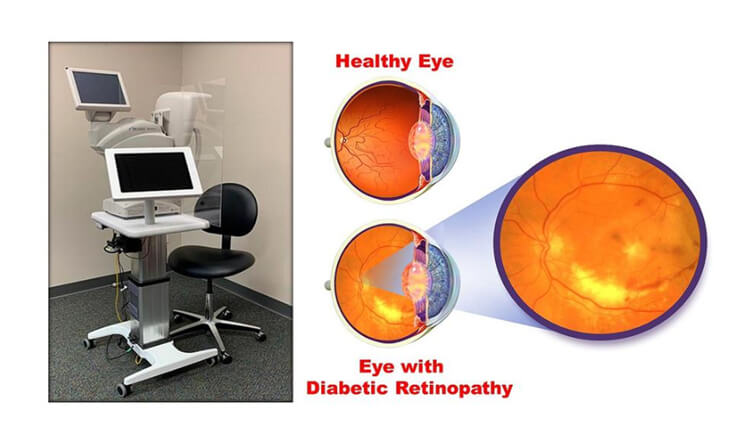
Ophthalmoscopy: Ophthalmoscopy uses a handheld instrument called an ophthalmoscope to examine the retina’s health. The ophthalmoscope has a light source and a magnifying lens that allow the doctor to see the back of the eye.
Dilated Eye Exam: To perform the dilated eye exam, your doctor will place drops in your eye to dilate your pupils. This allows the eye specialist in Delhi to see the inside of the eye, including the blood vessels, optic nerve, and retina.
Your doctor may take photographs of the eye’s interior to look for the following:
- Abnormalities in blood vessels and retina
- New blood vessels
- Retinal detachment
- Scar tissues
- Change in eye pressure
Fluorescein Angiography: In this test, your eye specialist in Delhi will put eye drops in your eyes to dilate your pupils and inject a dye called fluorescein into a vein in your arm. They will then take pictures of your eyes as the dye circulates through them.
This test helps the doctor determine which blood vessels are leaking fluid, have broken down, or have become blocked. The dye may leak into the retina or stain the blood vessels if they are abnormal. This information will help your doctor to create a tailored diabetic retinopathy treatment plan.
Optical Coherence Tomography (OCT): Optical coherence tomography (OCT) is a quick and painless eye test in which your doctor takes pictures of the back of your eye. It can be used to measure the thickness of the retina and look for cysts or swelling. OCT is similar to an ultrasound, but it uses light instead of sound waves to produce images.
During an OCT scan, a doctor will shine light into your eye. The light bounces back off the different layers of your retina, and the OCT machine creates a detailed image of each layer.
Slit Lamp Exam: Slit lamp exam uses a slit lamp, a microscope with high-intensity light, to examine the structure of the retina and the iris to rule out macular edema and neovascularization of iris.
Tonometry: Tonometry is a test that measures the pressure inside the eye. It is not a specific test for diabetic retinopathy, but it can be used to assess the risk of developing diabetic retinopathy and other eye diseases. If you have diabetic retinopathy and the intraocular pressure (IOP) is high, it may be a sign of another eye condition, such as glaucoma.
If you have diabetes, you should get regular comprehensive dilated eye exams to screen for diabetic retinopathy. Early detection and diabetic retinopathy treatment can help to prevent vision loss.

What is the Treatment for Diabetic Retinopathy?
Treatment for diabetic retinopathy depends on the severity of the condition and its stages. Mild diabetic retinopathy may not require treatment. However, it is essential to monitor your blood sugar levels closely and to get regular eye exams.
For moderate and severe diabetic retinopathy, your doctor may prescribe laser surgery, intravitreal injections, or vitrectomy (eye surgery), depending on the extent of the conditions.
Intravitreal Injections
Intravitreal injections deliver medications directly into the vitreous, the gel-like substance that fills the inside of the eye. Two types of intravitreal injections are used to treat diabetic retinopathy: anti-VEGF and steroidal.
ANTI-VEGF INJECTIONS
Anti-VEGF drugs work by blocking the action of vascular endothelial growth factor (VEGF), a protein that is involved in the growth of new blood vessels.
VEGF is a protein that plays a key role in blood vessel growth. In diabetic retinopathy, VEGF levels are elevated in the retina. This is due to a number of factors, including high blood sugar levels, lack of oxygen, and inflammation.
VEGF acts on endothelial cells, the cells that line the blood vessels. It causes these cells to multiply and grow new blood vessels, a process called angiogenesis. These blood vessels can leak blood and other fluids, causing swelling and damage to the retina. They can also become blocked, leading to ischemia (lack of blood flow).
Anti-VEGF injections block the effects of VEGF on endothelial cells and prevent the cells from multiplying and growing new blood vessels. They can help to reduce swelling, improve vision, and prevent serious complications such as retinal detachment and blindness.
Anti-VEGF injections are safe and effective; however, in rare cases, people may experience eye irritation and discomfort that subsides within a few days. These side effects can be controlled with eye drops. The different types of Anti-VEGF injections available in India are Bevacizumab (Avastin), Ranibizumab, Aflibercept and Brolucizumab. They vary in their efficacy, duration of action and cost.
Different types of anti-VEGF injections are used for diabetic retinopathy treatment.
- Ranibizumab (Lucentis): Ranibizumab is the most common intravitreal injection used to treat diabetic retinopathy by blocking VEGF. The frequency of injections depends on the severity of the condition and how well the patient responds to treatment. Injections are typically given every 4-6 weeks, and these intravitreal injections cost between 35,000 and 40,000 INR per injection.
- Brolucizumab (Pagenax): Brolucizumab is a newer anti-VEGF drug similar to ranibizumab but more potent and longer-lasting. One potential advantage of brolucizumab is that it may require fewer injections because of its 12-week duration of action.
- Aflibercept (Eylea): This anti-VEGF drug was originally developed for age-related macular degeneration (AMD) but is now used to treat diabetic retinopathy. It has a longer duration of action than other anti-VEGF drugs, lasting up to 8 weeks.
- Avastin: Avastin is an anti-VEGF drug that is approved to treat cancer, but it is also used off-label to treat diabetic retinopathy. It works similarly to Ranibizumab by blocking the action of VEGF in treating diabetic retinopathy. Avastin is usually less expensive than other anti-VEGF drugs; these intravitreal injections cost between 15,000 INR per injection.
STEROIDAL INJECTIONS
Steroidal injection reduces the inflammation and swelling in the retina, which can contribute to the progression of diabetic retinopathy. Sometimes, steroidal injections can cause cataracts or glaucoma, which is manageable. The most commonly used steriodal injection is a Dexamethasone implant known as Ozurdex. The effect of this implant lasts for 3-4 months and it costs around Rs 40-45000 per injection.
INTRAVITREAL INJECTION – PROCEDURE
Intravitreal injections are given in the hospital in sterile settings, generally the operation theatre. Your doctor will numb your eyes and eyelids with drops or gel, and sometimes, a small numbing injection is given. After that, your eye and eyelids will be cleaned, and an eyelid speculum is used to keep the eyelids open. Your doctor will ask you to look in a certain direction, and the medicine is injected into the white part of the eye with a very small needle. After the injection, the speculum is removed, and the eye is cleaned. The entire process takes about 10-15 minutes.
What to Expect After the Injection?
After the injection, you don’t need to follow any restrictions, except for avoiding potential eye contamination on the day of the injection. Intravitreal injections are safe without any side effects. However, in rare cases, patients can experience the following on the day of the procedure:
- Eye pain or discomfort
- Floaters
- Increased sensitivity to light
- Blurred vision
These side effects usually subside within two days. If they persist longer, contact your eye specialist in Delhi immediately.
Cost of Intravitreal Injections
The cost of intravitreal injections used for diabetic retinopathy can vary depending on several factors, including:
Type of Medication Used: Anti-VEGF and steroids are the two main types of medication used for diabetic retinopathy. Anti-VEGF injections are generally more expensive than steroidal injections.
The Number of Injections Required: The number of injections required will depend on the severity of the condition and the individual’s response to diabetic retinopathy treatment.
The Location of the Clinic: The location of the clinic significantly impacts the cost of infection. For example, a clinic in a major city may be more expensive than a rural area.
Expertise of the Doctor: The experience and knowledge of the doctor may also affect the cost of intravitreal injections. Usually, the eye specialist in Delhi with a proven track record charges more. However, the eyes are the vital organ of the body. Therefore, don’t compromise safety over cost.
While it is very complicated to estimate the cost of intravitreal injections without a diagnosis, consulting an eye specialist in Delhi can help you understand the procedure’s cost. Your doctor will also explain the injections’ benefits and possible risks.
Laser treatment
Laser treatment can help slow the progression of diabetic retinopathy by sealing off leaking blood vessels. This can help to prevent vision loss and improve vision in patients with diabetic retinopathy. Laser treatment is not painful but requires eye drops to numb the eye first. You will also see many bright flashes of light during the treatment. But these are temporary.
There are two types of laser treatment: focal laser photocoagulation therapy and scatter (pan-retinal) photocoagulation surgery.
Focal Laser Treatment (Photocoagulation): Focal laser treatment (photocoagulation) can help prevent vision loss from diabetic retinopathy by sealing off the abnormal blood vessels at macula. The heat from the laser causes scarring, which limits the growth of new blood vessels and reduces inflammation. This can help in reducing leakage from abnormal vessels and absorb excess fluid.
Scatter (pan-retinal) photocoagulation surgery (PRP): PRP treats proliferative diabetic retinopathy, the most advanced stage of diabetic retinopathy. This procedure involves making many tiny laser burns on the retina to shrink blood vessels and reduce the risk of bleeding. This is usually done in multiple sittings.
Laser treatment is usually performed as an outpatient procedure. Your eye specialist in Delhi will put numbing eye drops in your eyes. The laser is then used to make small burns in the retina. These burns seal off leaking blood vessels and prevent new blood vessels from growing.
The procedure typically takes 15-20 minutes to complete. You may experience some mild discomfort during the procedure, such as a feeling of pressure or warmth in the eye.
After the procedure, you may also experience some blurred vision, light sensitivity, and floaters. But there is no need to worry because these side effects are usually temporary and resolve within a few days.
Laser treatment for diabetic retinopathy may be done in one session or may require multiple sessions over time, depending on the severity of the condition.
The procedure is safe and painless; however, to recover quickly and safely, you must follow your doctor’s instructions, such as using eye drops and wearing eyeglasses for a few days after the procedure.
Vitrectomy Surgery
In the most severe stage of diabetic retinopathy, called proliferative diabetic retinopathy, abnormal blood vessels grow in the retina. These blood vessels can leak into the vitreous and form scar tissue, which can pull the retina away from the back of the eye. This can damage the retina and cause vision loss or blindness. In that case, your eye specialist in Delhi may recommend vitrectomy surgery to remove blood and scar tissue from the eye and replace the fluid to keep the retina in place.
Before the surgery begins, your surgeon will use eye drops and inject local anesthetic around the eye to numb it so that you don’t feel any pain or discomfort during the procedure. The injections are painless, and general anesthesia is rarely needed.
The surgeon will then make small openings in the eye wall and remove the cloudy vitreous humour from your eyeball. If necessary, the surgeon will then reattach or repair the retina. Finally, the surgeon will replace the vitreous fluid with a clear solution or gas bubble or silicon oil to restore the eye’s volume and keep the retina in place. Laser photocoagulation is also done to prevent further bleeding.
Vitrectomy surgery typically takes 1–2 hours, but it may take longer, depending on the complexity of the case. Vitrectomy surgery is an effective way to prevent vision loss from diabetic retinopathy and is recommended when other diabetic retinopathy treatments are unsuccessful. However, it is important to note that you should maintain your blood pressure, blood sugar level and cholesterol levels for an effective outcome. Uncontrolled diabetes can make the treatment less effective.
Note: If a person needs a vitrectomy in both eyes, the surgeon will only operate on one eye at a time. They typically wait until the patient has recovered from the first surgery before scheduling the second surgery.
After eye surgery, you can experience blurred vision, increased sensitivity to light and minor discomfort for a few hours. However, these side effects can be managed by following your doctor’s instructions, including wearing eyeglasses and using prescribed eye drops for the required time.

Take Away!
Diabetic retinopathy is a serious condition that can lead to blindness. However, with early detection and treatment, most diabetic retinopathy patients can maintain their vision. People with diabetes can also reduce their risk of developing diabetic retinopathy by controlling their blood sugar levels and having regular eye exams.
If you or your loved one are dealing with diabetic retinopathy, schedule your consultation with Dr Anisha Gupta, an eye specialist in Delhi. She will check your eye to determine the extent of the condition and prescribe the most appropriate diabetic retinopathy treatment.