Retina and Vitreous
The retina is the nerve tissue of the eye and is extremely important for the regular functioning of the eye. It is the eye’s light-sensitive area located at the back, and the vitreous is a gel-like substance in the eyeball. Both retina and vitreous may get diseased with age and with many body illnesses like diabetes, blood pressure and tuberculosis, requiring you to get retina surgery or retinal laser to avoid vision loss.
Dr Anisha Gupta is a retina specialist trained in numerous complex procedures. Under her care, you get sophisticated and effective treatment paths for any problem of the retina and vitreous.
When do you need retina surgery?
Experts in retina and vitreous diseases treat numerous conditions every day. Some standard treatments include the following.
Myopia and Myopic Retinal Problems
Myopia or near-sightedness or minus power glasses involve the eyeball being bigger, leading to the retina getting thinner. This may lead to retinal lattices, holes and tears in the periphery or outer area of the retina.
When left untreated, fluid from the vitreous enters these retinal holes or tears, causing retinal detachment. The retinal detachment can cause complete loss of vision, and requires major surgery to get back vision. In some cases, vision may be lost permanently.
The treatment for this condition involves photocoagulation or laser surgery to make burns around the tear, helping the retina combine with the underlying tissue. This procedure prevents the condition’s progression and retinal detachment from occurring.
Unfortunately, with most retinal tears, there are no severe symptoms. Therefore, patients do not realise the tear until the condition progresses to retinal detachment. Hence, it is important to get your retina checked annually by a retina specialist, if you are a myope.
Retinal Detachment Treatment
Retinal detachment occurs when the retina separates from the underlying choroid that supplies the blood to the retina. This leads to vision loss and potential permanent damage to the vision cells of the retina.
The symptoms of retinal detachment include:
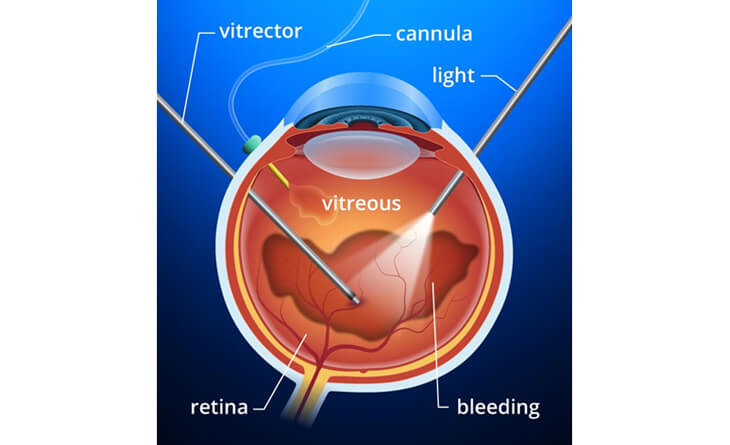
There are three kinds of retina surgery for retinal detachment:
Your vision takes time to improve, and you must rest for two weeks to promote a safer recovery. The final results and visual recovery depend on your macula’s condition and how long the detachment persisted before surgery.
Retina Surgery for Diabetic Retinopathy
Diabetic retinopathy happens when diabetes causes damages to the blood vessels at the retina. Its symptoms include:
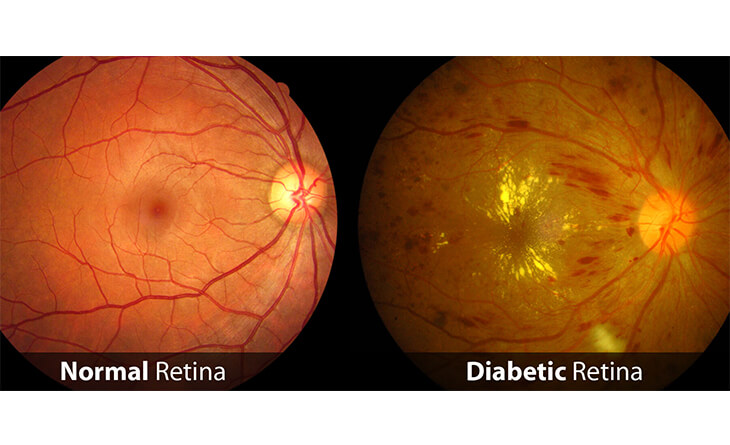
In the early stage, the retinal blood vessels’ walls weaken. This leads to fluid build-up and abnormal growth of new blood vessels, i.e. advanced retinopathy. The new vessels’ can cause a pull on the retina, eventually leading to retinal detachment, if left untreated.
Diabetic retinopathy is managed in different ways depending upon the stage and condition of the macula, including:
Since diabetes is a lifelong illness, there is no permanent solution to diabetic retinopathy. However, with an expert ophthalmologist like Dr Gupta, you can effectively treat it. A good diabetic control is also essential for recovery.
Vascular Occlusion Treatment
Vascular occlusion refers to blockages in the retina’s blood vessels, leading to fluid build-up. Its symptoms are similar to diabetic retinopathy, as is its treatment path.
Intravitreal injections and laser retina surgery are primarily used in treating vascular occlusion. Together, they help restore your eyesight, and prevent further vision loss.
Age-Related Macular Degeneration (AMD) Treatment
AMD happens when the macula in your retina’s centre gets affected with age. There are two types of AMD: dry and wet.
In dry AMD, the macula becomes thinner and yellow deposits (drusen) collect in the macula. In wet AMD, blood vessels grow under your macula and leak fluid into it. Both types can cause central vision loss as they advance.
Dry AMD does not need any treatment and progression is prevented through multivitamin or antioxidant supplements.
Wet AMD needs early and regular treatment to prevent vision loss. Intravitreal anti-VEGF injections are the mainstay of the treatment, initially needed on a monthly basis. Each eye needs a different number of injections and the treatment is generally long. There are also different types of injections, and your ophthalmologist chooses the best kind for your eye. These injections include:
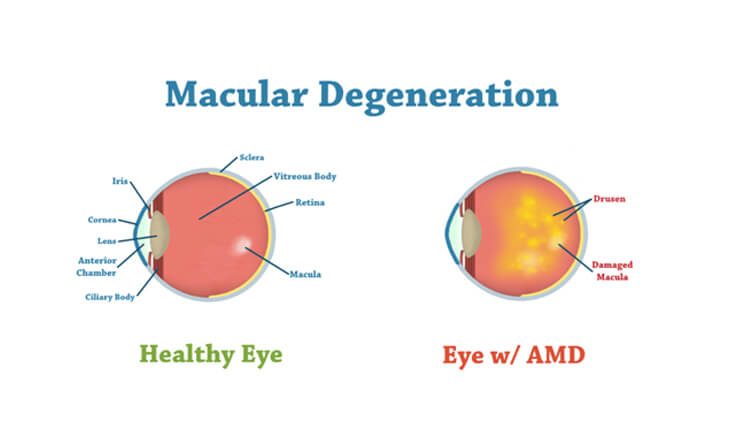
In some rare cases, laser is used on the wet AMD lesion. The laser seals off the abnormal blood vessels beneath the macula, stopping the leakage.
As a leading ophthalmologist in Delhi, Dr Gupta understands the nuances of different treatment paths and chooses the ideal one for you. Her solutions aim to minimise downtime and maximise vision, so your quality of life sees marked improvement.
Contact us for a consultation and get access to the latest techniques at the hands of an expert ophthalmologist today!
