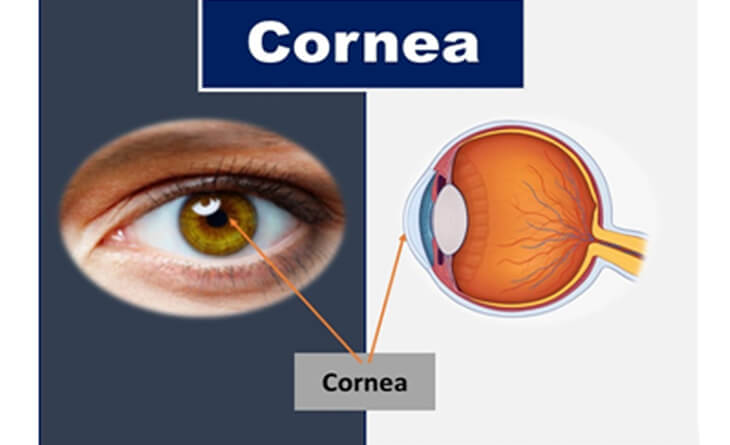
Cornea
The cornea is the outermost layer of the eye through which light enters, offering 70% of the eye’s focusing power. Thus, ensuring it stays healthy by regularly visiting a cornea specialist is imperative to preserve your vision.
Dr Anisha Gupta’s extensive expertise as a leading ophthalmologist enables her to treat a wide variety of corneal problems. She helps you optimise your eyesight with the latest technologies and techniques to maximise corneal health.
When do you need a cornea specialist?
The most common eyesight problems – refractive errors – happen due to improperly shaped corneas. While refractive errors are easily treatable with glasses, lenses, or surgery, there are also other corneal problems that experts regularly treat.
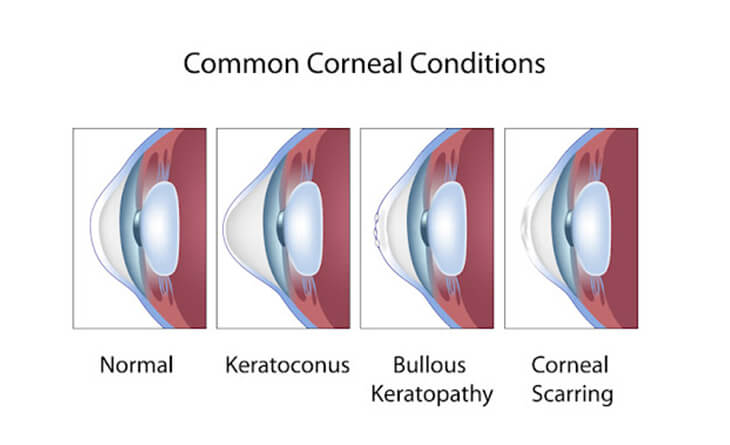
Keratoconus
Keratoconus is a disease in which the cornea distorts and develop a cone-shaped bulge, decreasing or changing vision. Its symptoms include:
Your cornea specialist manages mild or moderate keratoconus with the following treatments:
The keratoconus stage determines which treatment path is best-suited for your needs. With the right treatment, you get far better results and a more comfortable recovery.
Corneal Ulcer
A corneal ulcer involves an open sore/infection on the cornea. It generally occurs after an injury to the cornea. The cause can be bacterial, viral or fungal. The symptoms include:
Corneal ulcers are medical emergencies. If you experience any of these symptoms, you must go to a cornea specialist immediately. They offer the following treatments:
Corneal inflammation
Corneal inflammations can occur at any level inside the cornea. It may be superficial, stromal or endothelial. Most common cause of these is viral infections that lead to inflammation in the cornea. Its symptoms include:
Corneal inflammations require an early diagnosis and treatment by a cornea specialist for complete recovery and to avoid permanent scarring in the cornea. The treatments include oral antivirals, steroid eyedrops and lubricating eyedrops. You need to stay on a close follow up, so that your ophthalmologist can modify the treatment according to your response.
Corneal Dystrophies and Degenerations
Corneal dystrophies include a group of genetic conditions that turn the transparent cornea opaque. The most common dystrophies are macular corneal dystrophy, epithelial basement membrane dystrophy, and Fuchs corneal dystrophy. The symptoms include:
Depending on the type of dystrophy and the severity of the symptoms, your cornea specialist chooses one or more of the following treatment methods:
Corneal dystrophies progress gradually and often show no symptoms. The only way to catch and treat them is through regular eye checkups with your ophthalmologist. Catching this condition at the earliest stage enables a better recovery
Corneal Cancers
Corneal cancers are malignant tumours growing on the cornea. The most common types include squamous cell carcinoma, malignant melanoma and lymphoma. You should never ignore any growth on the eye.
The treatments offered by ophthalmologists include:
With an experienced cornea specialist like Dr Gupta, you can effectively catch and treat any malignant tumours as soon as possible.
Dry Eye
Dry eye happens when there is either decreased tear production or increased tear evaporation. Its symptoms include:
Dry eye treatment comes in the form of both medications and procedures. Depending on the cause behind your dry eye, you may need a combination of treatments, including lifestyle changes, that improve your corneal health.
Corneal Trauma
Eye trauma leads to either superficial corneal abrasion or full thickness corneal injury
Superficial corneal abrasion is very painful and needs early treatment with eye bandage or eyedrops, otherwise it can get infected leading to corneal ulcer formation and eventually blindness.
Full thickness corneal injury needs surgical repair of the cornea with sutures. This is also an emergency and should be treated as soon as possible otherwise the whole eye can get infected.
Hence, you should visit an Ophthalmologist immediately if you get an eye injury.
Corneal transplants or Keratoplasty
Cornea specialists are proficient in three main kinds of keratoplasty:
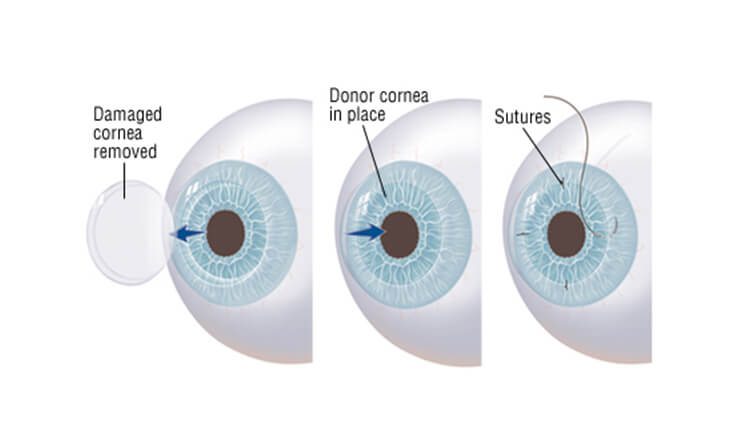
Recovering from your keratoplasty can take up to a year or longer as your eye adjusts to its new cornea. While your vision initially worsens, it gradually improves, and you can resume your normal daily activities. You may need steroid eye drops for several months to prevent rejection alongside other medications to keep infections and swelling at bay.
Improve your eye health exponentially with a leading ophthalmologist in Delhi. Contact Dr Anisha Gupta today!
